By NAHEEM NOAH
A Name from the Black Gap
Three months into constructing Carenector’s facility-to-facility platform, I acquired a name that crystallized the whole lot unsuitable with healthcare referrals. A hospital social employee, who was already utilizing our particular person affected person platform to assist households discover care, had been making an attempt to coordinate an institutional placement for an 82-year-old stroke affected person for six days. She’d made 23 cellphone calls. Despatched 14 faxes. The affected person was medically cleared however caught in an acute mattress costing $2,000 per day as a result of nobody might affirm which expert nursing amenities had open beds, accepted her Medicaid plan, and had stroke rehabilitation capability.
“I like what you constructed for sufferers,” she advised me, “however once I have to do a facility-to-facility switch, I’m again to faxing. Can’t you repair this workflow, too?”
She wasn’t unsuitable. We’re in 2025, and regardless of billions poured into well being IT and breathless AI guarantees, referring a affected person usually seems like stepping again into 1995. Earlier this year, THCB’s own editor Matthew Holt documented his attempt to navigate specialist referrals via Blue Protect of California. The echocardiogram referral his physician despatched by no means arrived on the imaging heart. When he wanted a dermatologist, his medical group referred him to a supplier who turned out to not be lined by his HMO plan in any respect. “There’s a big alternative right here,” Holt concluded after his odyssey via disconnected programs, “despite the fact that we’ve acquired now a number of the info…to combine it and make it helpful for sufferers.”
Clinicians make over 100 million specialty referrals yearly within the U.S., but research shows that as many as half are never completed.
Right here’s what we’ve discovered after a 12 months of operation: we constructed a consumer-facing platform that helps people and households discover care suppliers matching their wants, insurance coverage, and site—it now serves over 100 day by day customers, together with sufferers, social staff, and discharge planners. However fixing particular person care searches is just half the battle. The institutional referral workflow—hospital to expert nursing facility, SNF to rehab heart, clinic to specialist—stays trapped in fax machines and cellphone tag as a result of nobody redesigned the precise coordination course of.
That’s what we’re constructing now. And the query haunting us isn’t why we don’t have higher instruments? It’s why billions in AI funding left the institutional referral workflow just about unchanged?
The Structure of Failure
The reply isn’t about smarter algorithms or shinier dashboards. It’s a couple of elementary mismatch between how AI will get deployed and the way care coordination really works.
Begin with the info layer. One survey found that 69% of primary care physicians say they “always or most of the time” send full referral notes to specialists, but only 34% of specialists report receiving them. Even inside a single hospital system, info routinely vanishes at handoff factors. Matthew Holt skilled this firsthand when his physician’s referral for an echocardiogram merely by no means arrived on the imaging heart, regardless of prior authorization from Blue Protect already being within the system.
However the fragmentation goes deeper than lacking referrals. When Holt’s medical group referred him to a dermatologist, they despatched him to a supplier not lined by his HMO plan, despite the fact that the EMR had his insurance coverage info and member ID. As he documented, “there’s a big alternative right here…most of this knowledge about who I ought to go and see…is all obtainable. It’s simply not made very apparent in anybody place.” Medical teams, hospitals, and well being plans every preserve their very own programs, with no real-time integration to reply the straightforward query: Is that this supplier in-network for this affected person’s plan?
Then there’s the motivation drawback. A 2022 evaluation of CMS’s Comprehensive Primary Care Plus initiative discovered zero impression on care fragmentation. The researchers concluded that “excessive ranges of fragmented care persist” as a result of fee fashions don’t sufficiently reward suppliers for really closing referral loops. No person will get paid to chase down a misplaced referral, so referrals slip via the cracks.
Lastly, there’s the cussed analog actuality: over half of referral handoffs still happen by fax (56%) or paper handed to patients (45%). We haven’t rewired the workflow; we’ve simply digitized the mess.
Why “AI-Powered” Options Preserve Failing
Given these issues, you’d anticipate AI distributors to swoop in with options. As an alternative, most have made issues worse by treating AI as an add-on fairly than infrastructure.
The everyday method: OCR to scan paper referrals, auto-fill widgets for EHR fields, predictive algorithms for danger scoring. Every software solves a micro-problem whereas ignoring the macro-disaster. As one Innovaccer analysis put it, healthcare AI dangers “repeating previous errors, with disconnected instruments creating inefficiencies as a substitute of options.”
McKinsey’s recent analysis makes the identical level: the widespread adoption of AI-enabled level options “is creating a brand new fragmentation drawback.” The trail ahead isn’t extra remoted instruments however “assembling these capabilities right into a modular, linked AI structure.” And with out knowledge interoperability, none of this issues. As Innovaccer bluntly states, “With out clear knowledge, true interoperability is fantasy. With out interoperability, AI is simply costly noise.”
What We’re Constructing—Knowledgeable by 100+ Day by day Customers
Our shopper platform taught us one thing essential: if you give individuals (and the social staff serving to them) a software that truly matches their must obtainable suppliers in real-time, they use it. Day by day. Over 100 customers now depend on Carenector to navigate post-acute care, rehabilitation companies, and specialist referrals based mostly on their insurance coverage, location, and medical necessities.
However those self same social staff stored telling us, “This works nice once I’m serving to a member of the family search on their very own. However once I have to coordinate a hospital discharge or facility switch on behalf of my group, I’m again within the Stone Age.”
That’s why we’re now constructing the facility-facing platform, and we’re doing it otherwise than our first try. We’re not guessing at what hospitals want. We’re testing actively with a choose group of accomplice amenities, incorporating steady suggestions from their case managers and discharge planners who’ve seen what works within the shopper product.
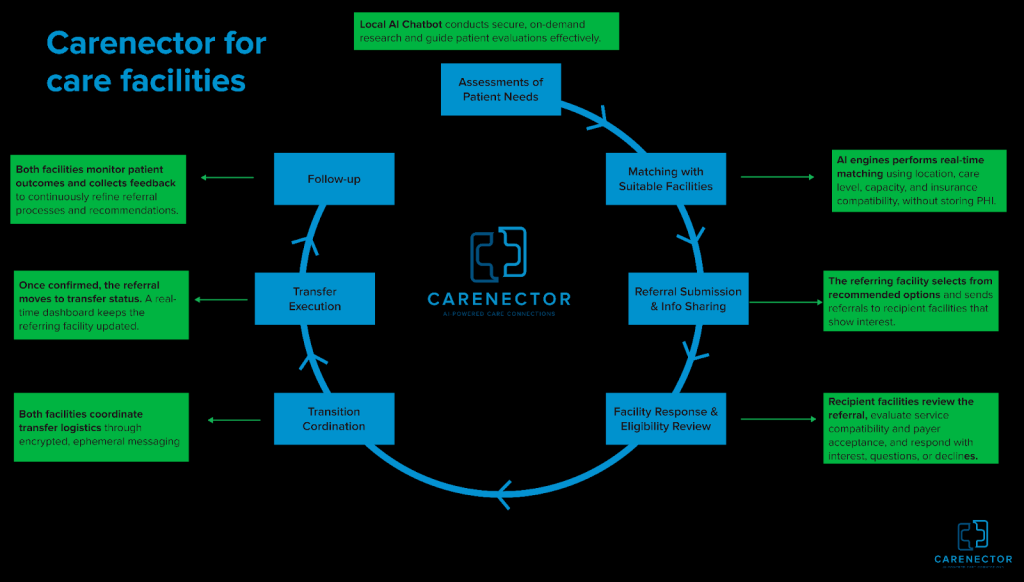
The Facility Workflow We’re Constructing
As an alternative of bolting AI onto present chaos, we’re rebuilding the institutional referral course of end-to-end. Care groups enter structured affected person wants—diagnoses, rehab necessities, tools, insurance coverage sort, location—with out sharing any personally identifiable info. No names, no medical file numbers, no birthdates within the preliminary matching section. Our AI engine performs real-time constraint-aware matching based mostly purely on medical and logistical standards: if a affected person wants expert nursing with PT companies, accepts solely particular Medicare plans, requires Spanish-speaking workers, and should be inside 10 miles, the system surfaces solely amenities assembly each criterion concurrently.
As soon as matches are discovered, referring amenities ship inquiries via safe channels with each side seeing the identical standing timeline. We’ve constructed ephemeral messaging threads the place nurses and consumption coordinators talk in real-time, no extra fax-into-void questioning. After a facility accepts, the whole lot stays in a single thread: transport scheduling, medicine reconciliation, and insurance coverage verification.
Right here’s what makes this clever: we monitor whether or not placements succeed or fail. Did the affected person get readmitted inside 30 days? Did the ability’s companies match what was promised? That final result knowledge feeds again into the matching algorithm, steadily studying which amenities ship on their commitments.
What We’re Studying in Actual-Time:
We’re constructing and testing the ability platform with a choose group of accomplice hospitals and expert nursing amenities. This isn’t broadly obtainable but. We’re iterating quickly based mostly on steady suggestions from these early adopters, and the teachings are reshaping our method:
- Belief requires transparency. Our early facility matching AI was a black field—”belief us, these are good matches.” Adoption amongst our pilot companions was horrible. Once we added transparency exhibiting why every facility matched based mostly on which particular standards, engagement jumped. Case managers wish to see the system’s reasoning, not simply its suggestions.
- Privateness is about good defaults, not paranoia. We initially constructed maximalist privateness controls that made the workflow clunky. Steady suggestions from our testing companions taught us the fitting method: begin with zero PII within the matching section, amenities see solely medical and logistical standards. Share affected person identifiers solely after a facility signifies curiosity and capability, utilizing expiring entry and audit logs. This center path eliminates the referral black gap (amenities can reply rapidly with out regulatory issues) whereas defending affected person privateness the place it issues most.
- The actual barrier isn’t know-how—it’s adoption technique. One social employee in our pilot stored faxing alongside our beta platform. Three weeks into testing, after seeing 4 profitable placements coordinated via our system, she stopped faxing. The tech didn’t change. Her confidence did. We’re studying to measure success not in options shipped however in workflows deserted.
Past Expertise: What the System Wants
Even the best-designed AI received’t repair referrals alone. The ecosystem wants parallel adjustments:
- Regulatory reform: CMS might require digital referral monitoring as a situation of participation and pay suppliers for profitable referral completion, not only for encounters.
- Requirements adoption: FHIR APIs and HL7 interoperability requirements exist however stay optionally available. Necessary adoption would let totally different distributors’ programs really speak to one another.
- Shared accountability: The largest cultural shift wanted is shifting from “I despatched the referral” to “I confirmed the affected person acquired care.” ACOs and value-based contracts are nudging this route, however slowly.
From Band-Aids to Rebuilt Plumbing
That 82-year-old stroke affected person? She acquired positioned on day seven via the social employee’s fax machine. The delay value the hospital $14,000 in extra acute care days. Multiply that throughout tens of millions of referrals yearly and also you glimpse the financial waste embedded in our infrastructure.
The know-how to repair this exists—real-time knowledge pipelines, constraint satisfaction algorithms, safe messaging, final result analytics. What we haven’t had is the need to reassemble these items into coherent workflows as a substitute of piling them onto damaged processes.
Our shopper platform proved that if you rebuild the search and matching layer from scratch, individuals undertake it. Now we’re testing whether or not the identical method works for institutional coordination with a choose group of pilot amenities. The early alerts from these companions are promising, case managers who use each our merchandise inform us the ability platform seems like a pure extension of what they already belief.
The toughest conversations aren’t with engineers, they’re with hospital directors who’ve been burned by “AI options” that promised transformation and delivered costly shelfware. We don’t lead with AI anymore. We lead with a query: When your case supervisor sends a referral, do they know—with certainty—that it was acquired, reviewed, and acted on? For many hospitals, the reply is not any. That’s the issue we’re fixing with our pilot companions.
If we succeed, it received’t be as a result of we constructed a better algorithm. It’ll be as a result of we rebuilt the plumbing based mostly on what actual customers advised us they wanted. And if we fail? It’ll in all probability be as a result of we forgot that know-how isn’t the toughest a part of healthcare—belief is.
Naheem Noah is a PhD researcher on the College of Denver and co-founder of Carenector, a healthcare referral platform.
